 It is common for elderly people to undergo changes in their circulatory system. This can be a normal part of the aging process as a result of strain on the veins and arteries. Some of the symptoms that are associated with poor circulation include a tingling sensation, pain, and muscle cramps. Additionally, the feet may turn blue or purple, the toenails can become weak, and there can be hair loss on the legs. Mild relief can be found by massaging the feet, staying active, and it can help to refrain from drinking caffeine and alcohol. Poor circulation may be a symptom of an underlying condition. If you have signs of this ailment, it is strongly suggested that you speak with a podiatrist as quickly as possible who can properly assess and treat your circulation issues.
It is common for elderly people to undergo changes in their circulatory system. This can be a normal part of the aging process as a result of strain on the veins and arteries. Some of the symptoms that are associated with poor circulation include a tingling sensation, pain, and muscle cramps. Additionally, the feet may turn blue or purple, the toenails can become weak, and there can be hair loss on the legs. Mild relief can be found by massaging the feet, staying active, and it can help to refrain from drinking caffeine and alcohol. Poor circulation may be a symptom of an underlying condition. If you have signs of this ailment, it is strongly suggested that you speak with a podiatrist as quickly as possible who can properly assess and treat your circulation issues.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Bruce Smit, DPM of Frankfort Foot & Ankle Clinic. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
 Blisters on the feet can be uncomfortable, painful, and if infected, can become a serious health issue. Blisters are a small pocket of fluid that develops over a damaged portion of skin. This is the body’s natural defense in protecting the area as new skin forms. Blisters can develop from wearing shoes that do not fit correctly, and this can cause the foot to rub against the shoe. Many patients find it helpful to keep their feet as dry as possible, and this can aid in preventing blisters. Additionally, blisters can develop from a severe sun or chemical burn, frostbite, or possibly from an allergic reaction. If you have developed blisters on your feet, it is suggested that you speak to a podiatrist who can guide you toward proper treatment and healing techniques.
Blisters on the feet can be uncomfortable, painful, and if infected, can become a serious health issue. Blisters are a small pocket of fluid that develops over a damaged portion of skin. This is the body’s natural defense in protecting the area as new skin forms. Blisters can develop from wearing shoes that do not fit correctly, and this can cause the foot to rub against the shoe. Many patients find it helpful to keep their feet as dry as possible, and this can aid in preventing blisters. Additionally, blisters can develop from a severe sun or chemical burn, frostbite, or possibly from an allergic reaction. If you have developed blisters on your feet, it is suggested that you speak to a podiatrist who can guide you toward proper treatment and healing techniques.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Bruce Smit, DPM of Frankfort Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters are a common ailment of people who wear shoes that are either too tight or rub against the feet in an uncomfortable way. Knowing the basics of blisters is important for understanding how they are formed and what treatments should be used for them.
A blister on the foot, or any other part of the body, is a small pocket that is filled with fluid. It usually forms on the upper layer of the skin because these layers are loose enough to allow a blister to form. The most common fluid in a blister is just a clear, watery-like fluid that usually isn’t cause for concern. However, blisters can fill up with blood if they are deep enough and pus if they have become infected with bacteria.
Blisters almost always form on the feet due to shoes rubbing up against the foot, where the friction causes blisters. These can occur after you have walked for a long period of time or when your shoes do not fit you properly. Your feet are also more prone to blisters if they are moist, so keeping them dry and clean is one preventative step you can take.
Preventing infection should be the number one concern when treating blisters, as well as relieving the pain they can cause. Using a bandage to cover up the blister will help it heal and prevent bacteria from entering it. New skin will form under the blister and eventually cause it to pop. You can also take a sterilized pin and try to pop it yourself.
If the blister is filled with pus or blood, seeking treatment from a doctor is ideal. Antibiotics may need to be taken in order to completely eliminate the bacteria inside the blister. See a doctor to have an antibiotic prescribed.
The best way to treat blisters is to prevent them all together. Keeping your feet dry and making sure that your shoes fit properly are just two of the steps you can take to prevent blisters. Shoes that are too tight or shoes that are too loose and allow your feet to slide in them will cause blisters. Applying a bandage to an area where you think a blister is about to form is another way you can prevent them.
The arch is the curved area in the center sole of the foot. At birth, babies do not have arches in their feet, but most will develop arches over time. Those who don’t develop arches have congenital flat feet, which are usually asymptomatic. It is also possible to develop arches normally and then lose them over time for a variety of reasons. This is known as acquired flat feet, and is often accompanied by foot pain or discomfort. But why do we have arches in the first place? The arch of the foot is a very useful structure. It helps the feet stand, stay balanced, run, walk, and jump by adding flexibility and springiness to the foot. With an arch, the foot is better able to absorb shock from physical activities, and the body’s weight is more evenly distributed around the surface of the foot. If you have flat feet and are experiencing any foot pain, please seek the care of a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Bruce Smit, DPM from Frankfort Foot & Ankle Clinic. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
If standing or walking for long periods causes a pain on the outside of your ankle, you may have sinus tarsi syndrome. The sinus tarsi is a kind of tunnel between two other foot bones that contains ligaments, muscle, nerves, blood vessels and fat. When it gets pinched, it causes pain in front of and below the pointy bone on the outside of your ankle, which is actually the end of the fibula. Swelling and pain when rotating your foot outward are also symptoms. Sinus tarsi syndrome is common in people who have previously sprained an ankle. Non-operative treatments include stopping the activity that is causing the pain, wearing more comfortable shoes and an ankle brace, taking non-steroidal anti-inflammatory medication, and getting corticosteroid injections. An X-ray or digital imaging test from a podiatrist is suggested for a full examination and diagnosis of your foot and ankle.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Bruce Smit, DPM from Frankfort Foot & Ankle Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The ankle joint is the point at which the bones of the leg and foot join. This joint is crucial because it is responsible for the foot’s mobility. Ankle pain is typically the result of inflammation from an injury to bones, joint space, cartilage, ligaments, tendons, or muscles in the area. Commonly associated symptoms with ankle pain are bruising, redness, numbness, stiffness, weakness, and tingling.
The most common causes of ankle pain are sprains and injuries. Ankle sprains are one of the most common musculoskeletal injuries. Sprains occur when the ligaments of the ankle become partially or completely torn due to sudden stretching. Sprains can occur on either the inner or outer sides of the ankle joint. Usually, these injuries occur when the ankle is twisted in an activity by stepping off an uneven surface. More specific causes include rheumatoid arthritis, gout, osteoarthritis, and Achilles tendonitis.
If you are experiencing ankle pain, you should consult with your podiatrist to choose the best method of care. Your doctor will conduct an examination of your ankle to determine the underlying cause of the pain.
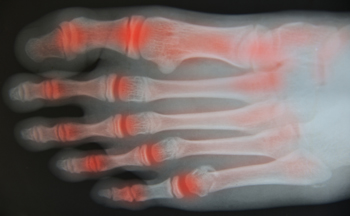 Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Bruce Smit, DPM of Frankfort Foot & Ankle Clinic. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.